
Keloid scarring is a concern that often causes hesitation for people considering a hair transplant. Because the procedure involves thousands of small incisions to the scalp, patients who have experienced abnormal scarring in the past may worry that a hair transplant could trigger raised, thick, or permanent scars. These concerns are understandable, especially for individuals who have developed keloids after piercings, surgery, or skin injuries.
The good news is that keloid formation after a hair transplant is rare. Most patients heal with minimal scarring, particularly when modern techniques such as FUE or DHI are used. However, the risk is not zero. Keloids are the result of an exaggerated healing response, and in people who are genetically predisposed, even small wounds can sometimes lead to excessive scar tissue. This makes careful assessment and surgical planning essential before proceeding with any hair restoration procedure.
This article explains how keloid scarring relates to hair transplant surgery, who may be at higher risk, how surgeons assess and reduce that risk, and when a hair transplant may not be recommended. By understanding these factors, patients can make informed decisions and avoid unnecessary complications while protecting both scalp health and long-term results.
What Is a Keloid Scar?
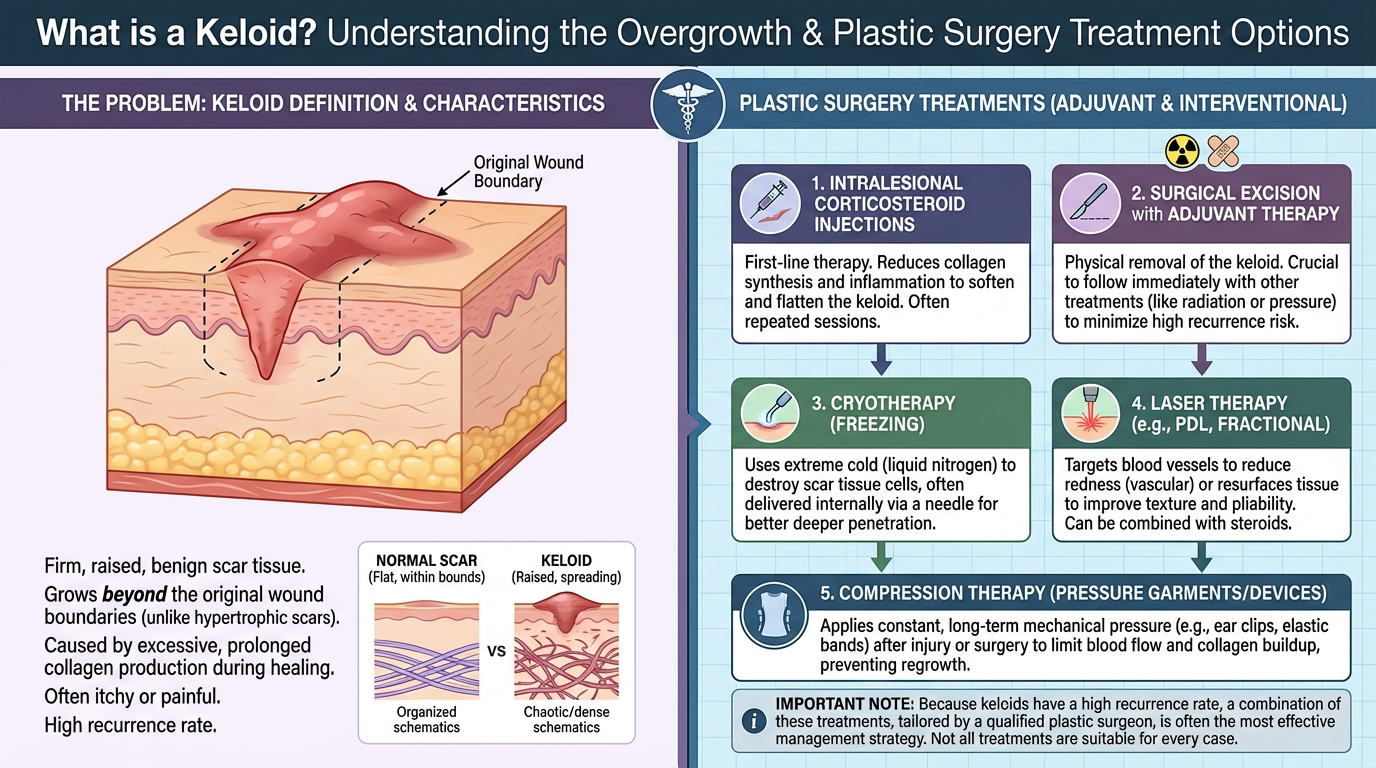
A keloid scar is an abnormal type of scar that forms when the body produces excess collagen during the healing process. Instead of stopping once a wound has closed, scar tissue continues to grow beyond the original injury, creating a raised, thick, and sometimes firm scar that extends into the surrounding skin.
Unlike normal scars, keloids do not gradually flatten or fade over time. They can remain permanently elevated and may continue to enlarge months or even years after the initial skin injury. In some cases, keloids are associated with itching, tenderness, tightness, or cosmetic discomfort, especially when they develop in visible areas.
Common characteristics of keloid scars include:
- Thick, raised, and firm texture
- Growth beyond the original wound edges
- Smooth or shiny surface appearance
- Color ranging from pink or red to dark brown, depending on skin type
- Persistence without natural regression

Why Keloid Scarring Is Important in Hair Transplant Surgery
Hair transplant surgery involves creating hundreds to thousands of tiny incisions in the scalp, both in the donor area where follicles are extracted and in the recipient area where they are implanted. For most patients, these micro-injuries heal smoothly and leave little to no visible scarring. However, in individuals prone to abnormal wound healing, these same incisions can trigger excessive scar formation.
Keloid scarring is particularly relevant in hair transplantation because the scalp is a visible area and because scarring can affect both cosmetic outcomes and future treatment options. If abnormal scar tissue develops in the donor area, it can reduce flexibility for additional procedures and may create visible texture or elevation that is difficult to conceal with hair.
Key reasons keloid risk must be evaluated before a hair transplant include:
- Multiple micro-incisions increase overall wound exposure
- Donor area scarring can affect future transplant options
- Raised scars may remain visible even with surrounding hair
- Abnormal healing can compromise aesthetic harmony
- Early prevention is more effective than post-scar treatment
The different types of scarring that can occur after hair transplant surgery and how they affect long-term appearance are explained in our article Hair Transplant Scars: What You Need to Know.
Can Hair Transplants Cause Keloid Scars?
In clinical practice, keloid scarring after a hair transplant is rare. Most patients heal with minimal or invisible scarring, particularly when modern techniques are used and the scalp does not have a history of abnormal wound healing. This is why hair transplantation is generally considered safe from a scarring perspective for the majority of candidates.

Risk increases only when the body’s healing response is predisposed to overreact. In patients who form keloids easily, even minor skin trauma can stimulate scar tissue that extends beyond the original wound. In such cases, the concern is not whether hair transplantation is technically safe, but whether the individual’s skin is likely to respond in an abnormal way.
Rather than assuming that hair transplants cause keloids, it is more accurate to understand that:
- The procedure does not create keloids in healthy-healing skin
- Keloids develop due to individual biological response
- Modern incision techniques significantly reduce overall risk
- Proper screening is more important than the technique alone
Who Is at Higher Risk of Keloid Scarring?
Keloid scarring does not develop randomly. Certain individuals have a higher biological tendency to form excessive scar tissue, and identifying this risk is one of the most important steps before planning a hair transplant.
Groups commonly considered higher risk include:
- Individuals with a documented history of keloid scars
- Patients who developed raised scars after minor procedures
- People with family members prone to keloid formation
- Those whose scars tend to grow beyond the original wound
- Patients with unpredictable or prolonged wound healing
Keloid Risk in Donor Area vs Recipient Area
Keloid risk in hair transplant surgery is not evenly distributed across the scalp. The donor area and the recipient area differ in skin thickness, tension, blood supply, and healing behavior, all of which influence how scars form.
The differences in healing behavior, incision depth, and long-term impact between these two areas are summarized clearly in the table below:
| Keloid Factor | Donor Area | Recipient Area |
|---|---|---|
| Skin tension | Higher | Lower |
| Number of incisions | High due to graft extraction | High but more dispersed |
| Incision depth | Deeper with follicle removal | Shallower placement sites |
| Visibility of scars | More noticeable if hair is short | Often concealed by transplanted hair |
| Impact on future procedures | May limit further extraction | Less effect on future options |
| Overall keloid concern | Moderate to higher in predisposed patients | Lower but not negligible |
The role of the donor area in long-term outcomes and why its condition must be protected is explained in our article Hair Transplant Donor Area: Why It’s Critical for Natural and Lasting Results.
Hair Transplant Techniques and Keloid Risk
The choice of hair transplant technique plays an important role in how the scalp heals, especially for patients with a higher risk of abnormal scarring. While no technique can completely eliminate keloid risk in predisposed individuals, modern methods are designed to minimize skin trauma, control incision depth, and promote more predictable healing.
The differences between commonly used hair transplant techniques and their relationship to keloid risk are outlined below:
| Technique | Incision Characteristics | Level of Skin Trauma | Keloid Risk Consideration |
|---|---|---|---|
| FUE (Follicular Unit Extraction) | Small circular extraction sites | Low to moderate | Lower risk than larger incisions when evenly distributed |
| Sapphire FUE | Ultra-fine, precise incisions with sapphire blades | Low | Improved control of incision size may support smoother healing |
| DHI (Direct Hair Implantation) | Direct implantation with minimal surface incisions | Very low | Reduced surface trauma may be beneficial for sensitive skin |
| FUT (Strip Method) | Single linear incision in donor area | Higher | Linear scar carries higher concern in keloid-prone patients |
How Surgeons Approach Keloid Risk Before a Hair Transplant
For surgeons, keloid risk assessment is less about labeling a patient as “high” or “low” risk and more about deciding how much surgical stress the scalp can safely tolerate. From a surgical perspective, this approach typically includes:
- Deciding whether surgery is appropriate at all: In some cases, the safest decision is postponement or avoidance rather than modification
- Controlling total wound burden: Limiting graft numbers and avoiding concentrated extraction zones to reduce cumulative trauma
- Choosing the least invasive technique: Favoring methods that minimize incision depth and surface disruption
- Adjusting density and spacing: Lower implantation density may be used to allow calmer healing
- Prioritizing donor preservation: Protecting the donor area from aggressive extraction that could lead to raised or visible scars
- Planning for reversibility: Ensuring that any decision made does not permanently compromise future options
The importance of surgical planning, donor management, and controlled technique selection for achieving reliable outcomes is discussed further in our article Hair Transplant Success: The Key Elements Behind a Great Result.
What Happens If a Keloid Forms After a Hair Transplant?
If a keloid begins to form after a hair transplant, it usually develops gradually rather than appearing suddenly. Early changes may include localized firmness, raised skin texture, persistent redness, or thickening around extraction or implantation sites. These signs are often subtle at first, which is why early follow-up and monitoring are important.
When a keloid is suspected, the response focuses on medical management rather than surgical correction. Common approaches include:
- Early use of anti-inflammatory treatments to calm excessive tissue response
- Local therapies aimed at limiting further scar growth
- Close observation to track progression rather than immediate intervention
- Avoidance of additional trauma to the affected area
Guidance on gentle aftercare, inflammation control, and protecting the scalp during healing is covered in our article Hair Care After Hair Transplant: Products That Support Recovery and Growth.
When a Hair Transplant Is Not Recommended
In some cases, the risk of keloid formation outweighs the potential benefits of hair transplant surgery. When the likelihood of abnormal scarring is high, proceeding with surgery can lead to permanent cosmetic issues and limit future treatment options. In these situations, avoiding surgery is often the safest and most responsible decision.

A hair transplant is generally not recommended when:
- There is a clear history of aggressive keloid formation after minor skin injuries
- Active or growing keloids are present on the scalp, donor area, or nearby regions
- Previous surgical scars have expanded beyond the original wound edges
- Healing responses have been unpredictable or progressively worsened over time
- The donor area shows signs of abnormal thickening or scar sensitivity
- The potential cosmetic risk outweighs the expected benefit of hair restoration
Keloid Risk Management for Your Hair Transplant in Turkey with MCAN Health
Keloid risk requires a careful and responsible approach to hair transplant planning. While most patients heal normally, those with a tendency toward abnormal scarring need additional evaluation, conservative decision-making, and realistic guidance. A successful outcome in these cases depends less on graft numbers and more on respecting how the skin heals over time.

At MCAN Health, keloid risk is approached as part of overall surgical responsibility rather than a technical obstacle to work around. Each patient is assessed with a focus on long-term scalp health, donor area preservation, and avoidance of unnecessary trauma. When risk is present, surgical plans are adjusted or postponed to prevent permanent cosmetic complications.
When you choose MCAN Health for your hair transplant in Turkey, you benefit from:
- Careful pre-operative screening that evaluates scar history, skin behavior, and healing patterns
- Conservative surgical planning designed to minimize tissue stress and incision load
- Technique selection based on healing behavior, not routine preference
- Ethical decision-making, including advising against surgery when risk outweighs benefit
- Close post-operative monitoring to detect and manage abnormal healing early
Hair transplantation should never come at the cost of long-term scalp damage. By prioritizing patient safety, controlled planning, and transparent guidance, MCAN Health helps ensure that hair restoration decisions are made responsibly, with lasting results and minimal risk.
 Hair Transplant and Scalp Psoriasis: Is It Safe, Effective, and Who Qualifies?
Hair Transplant and Scalp Psoriasis: Is It Safe, Effective, and Who Qualifies?  Can You Drink Alcohol After a Hair Transplant? Timing and Risks Explained
Can You Drink Alcohol After a Hair Transplant? Timing and Risks Explained  Hair Transplant Turkey vs USA: Cost, Quality, Results, and Safety Compared
Hair Transplant Turkey vs USA: Cost, Quality, Results, and Safety Compared