
Scalp psoriasis is a common concern among people considering a hair transplant. The condition causes patches of redness, scaling, and inflammation on the scalp, and these symptoms often raise questions about whether surgery is safe, effective, or even possible. Many patients worry that psoriasis might damage hair follicles, interfere with healing, or affect graft survival. Others want to know if a hair transplant could trigger additional flare-ups.
The reality is that scalp psoriasis does not automatically rule someone out as a candidate for a hair transplant. With the right evaluation and good disease control, many patients achieve successful and natural-looking results. However, psoriasis requires careful planning because the scalp can be more sensitive, and flare patterns can influence timing and technique.
This article explains how psoriasis affects the scalp, who qualifies for a hair transplant, what risks need to be considered, and how experienced surgeons manage these challenges. It provides clear guidance to help patients understand when surgery is appropriate and how to prepare for the best possible outcome.
What Is Scalp Psoriasis?
Scalp psoriasis is a chronic autoimmune condition that speeds up the skin cell cycle, causing thick, scaly patches to form on the scalp. These patches may appear as white, silvery, or red areas that can itch, flake, or feel tender. Psoriasis is not contagious, and it does not directly damage the hair follicles themselves. Instead, the inflammation affects the skin that surrounds them.
The condition typically follows a cycle. Patients experience periods of flare-ups when symptoms become more visible and moments of remission when the scalp looks and feels relatively normal. Flare intensity varies widely from person to person, and this variability is an important factor when considering a hair transplant.
Although psoriasis often looks severe, the impact on hair growth is usually temporary. Shedding can occur during flare-ups due to irritation, scratching, or the weight of thick plaques, but the follicles remain capable of producing new hair once the inflammation settles.
Patients who experience psoriasis-related shedding often confuse it with other forms of hair loss. Understanding the differences can be helpful, and our guide What Is Diffuse Thinning? Can a Hair Transplant Fix It? explains how diffuse thinning behaves compared to temporary shedding caused by inflammation.

How Scalp Psoriasis Affects the Hair and Scalp
Scalp psoriasis does not permanently damage hair follicles, but the inflammation it causes can influence how the scalp behaves during flare-ups and how hair temporarily appears. These effects are important to understand when evaluating suitability for a hair transplant:
- Inflammation around follicles: The skin becomes irritated, red, and sensitive, which can make the scalp less comfortable during healing.
- Temporary shedding: Scratching, plaque buildup, or inflammation can loosen hairs, but the follicles remain capable of regrowth.
- Thick plaques pulling on hair: Heavy scaling can add tension to strands and contribute to temporary thinning.
- Increased scalp sensitivity: Some patients experience tenderness, making the scalp slightly more reactive after surgical procedures.
- Variable flare patterns: Psoriasis may be mild and occasional or severe and frequent, which affects when and how a hair transplant should be scheduled.
To see how psoriasis affects the deeper structures of the hair follicle, you may find our article Hair Structure Diagram Explained: Layers, Follicles, and How Hair Actually Grows especially insightful.
Can You Get a Hair Transplant If You Have Scalp Psoriasis?
Many people with psoriasis worry that the condition automatically disqualifies them from receiving a hair transplant. In reality, a transplant can be safe and effective, but only under the right conditions. The key factor is whether the psoriasis is currently active or well controlled.
You can qualify for a hair transplant if:
- Your psoriasis is in remission with no active plaques in the donor or recipient areas.
- Your flare-ups are infrequent or mild.
- Your scalp skin appears stable, calm, and healthy before surgery.
- Your dermatologist confirms that the condition is managed and stable.
A transplant is not recommended when:
- Psoriasis is active on the scalp during the planning phase.
- Flare-ups are frequent, severe, or unpredictable.
- Thick plaques cover large areas of the donor or recipient zones.
Risks of Hair Transplantation in Patients With Psoriasis
A hair transplant can still be successful for patients with psoriasis, but the condition introduces specific risks that must be understood before planning surgery. These risks depend on whether the condition is active, how sensitive the scalp is, and how the skin responds to trauma.
The key risks for psoriasis patients undergoing hair transplantation are indicated on the table below:
| Risk | What It Means | Why It Matters |
|---|---|---|
| Koebner Phenomenon | Psoriasis lesions may appear in areas of skin trauma. | Incisions made during transplantation can trigger new plaques. |
| Increased Inflammation | The scalp becomes more reactive or irritated during healing. | Can slow recovery and create discomfort or redness. |
| Higher Chance of Shock Loss | Temporary shedding of native hair near the transplant site. | Inflamed skin is more vulnerable, increasing shedding risk. |
| Scalp Sensitivity | Psoriatic skin may react more strongly to surgical tools and post-op products. | Can affect comfort and tolerance to the procedure. |
| Slightly Higher Infection Risk | Active psoriasis weakens the skin barrier. | Openings in unhealthy skin may have higher infection risk. |
Who Is a Good Candidate for a Hair Transplant With Psoriasis?
Not every patient with scalp psoriasis is automatically excluded from hair transplantation. The key factor is how well the condition is controlled. Candidates are evaluated based on scalp health, flare frequency, and overall stability of the disease.
Patients who typically qualify include:
- Those in long-term remission: A calm, plaque-free scalp indicates that the skin can heal normally after surgery.
- Individuals with mild or localized psoriasis: Small, manageable patches outside the donor and recipient zones are usually acceptable.
- Patients with clear donor and recipient areas: Hair transplantation should only be performed on skin that shows no active inflammation.
- People with stable medical management: Patients using topical treatments, systemic medications, or biologics with good control are often suitable.
- Individuals who understand healing expectations: Psoriasis patients may require slightly longer recovery times and closer follow-up.
When a Hair Transplant with Psoriasis Is Not Recommended
Even though many patients with psoriasis can successfully undergo a hair transplant, there are situations where the procedure is not advisable. Operating on an unstable or actively inflamed scalp increases the risk of complications, poor healing, and reduced graft survival.
A hair transplant is generally not recommended when:
- Psoriasis is in an active flare-up: Redness, plaques, or scaling on the scalp signal inflammation that can disrupt healing.
- Lesions cover the donor or recipient areas: Transplanting into diseased skin decreases graft survival and increases the risk of Koebner phenomenon.
- Flare-ups occur frequently or unpredictably: Unstable psoriasis can interfere with postoperative recovery and long-term results.
- The patient shows strong Koebner reactions: If minor skin trauma often triggers new plaques, transplant incisions may do the same.
- The donor area is weakened: Chronic inflammation may temporarily thin donor hair or make extraction more difficult.
- Systemic disease is uncontrolled: Patients still searching for effective medical treatment should stabilize their condition before considering surgery.
How to Prepare for a Hair Transplant If You Have Psoriasis
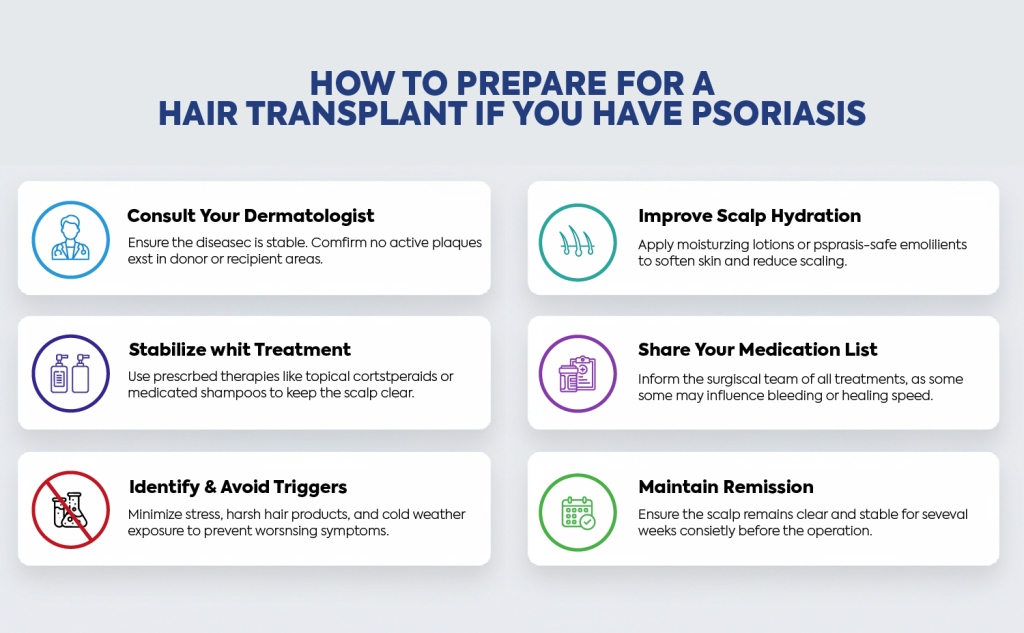
Proper preparation is essential for ensuring safe surgery and smooth healing. For patients with psoriasis, the goal is to calm the scalp, minimize inflammation, and create the healthiest possible environment for graft survival.
Key preparation steps include:
- Consult your dermatologist: Medical clearance ensures the disease is stable and that no active plaques are present in critical areas.
- Stabilize with treatment: Use prescribed therapies such as topical corticosteroids, medicated shampoos, or systemic treatments to keep the scalp clear before surgery.
- Identify and avoid triggers: Stress, harsh hair products, cold weather, and certain shampoos can worsen psoriasis and should be minimized before the procedure.
- Improve scalp hydration: Moisturizing lotions or psoriasis-safe emollients can help soften the skin and reduce scaling.
- Share your medication list with the clinic: Some psoriasis treatments may influence bleeding, healing speed, or immune response, so your surgical team must be informed.
- Maintain remission for several weeks: Surgeons prefer operating when the scalp has remained clear and stable for a consistent period.
How Hair Transplant Surgery Is Performed for Psoriasis Patients
For patients with psoriasis, a hair transplant must be performed with extra precision and sensitivity. The goal is to minimize trauma to the scalp, avoid triggering flare-ups, and ensure that grafts are placed into healthy, stable skin. While the overall procedure is similar to a standard FUE-based transplant, several adjustments are made to protect the scalp.
Key considerations during surgery
- Operating only on clear skin: Surgeons avoid any area showing plaques, redness, or active irritation.
- Gentle handling of the scalp: Reduced trauma helps prevent the Koebner phenomenon and improves comfort during healing.
- Careful selection of technique:
- FUE Hair Transplant is commonly preferred because it creates minimal surface trauma.
- Sapphire FUE can offer smooth, precise incisions that may be better tolerated.
- DHI Hair Transplant allows controlled implantation without creating larger incisions, which benefits sensitive scalps.
- Adjusted incision depth and spacing: The surgeon may lower density or modify the angle in areas prone to irritation to allow better healing.
- Constant evaluation during the procedure: Surgeons monitor the skin’s response to ensure the transplant site remains calm and stable.
For a full overview of what happens during a typical transplant from start to finish, our guide Hair Transplant Operation: A Detailed Look at Every Stage of Your Surgery in Turkey provides a clear breakdown of each step.
Recovery Expectations for Psoriasis Patients
Recovery from a hair transplant can be slightly different for patients with psoriasis. While most individuals heal normally, the scalp may respond more sensitively, and flare management becomes an important part of the healing process. The table below outlines what patients can typically expect during recovery:
| Aspect of Recovery | What to Expect | Why It Matters |
|---|---|---|
| Healing Speed | Healing may be slightly slower than average. | Psoriatic skin can take more time to settle after minor trauma. |
| Inflammation | Mild redness or sensitivity may last longer. | The immune system is more reactive in psoriasis patients. |
| Flare-Up Risk | A small chance of temporary flare near the transplant site. | Stress, trauma, or healing processes can trigger inflammation. |
| Shock Loss | Slightly higher chance compared to non-psoriasis patients. | Inflamed or sensitive skin may shed more native hairs temporarily. |
| Aftercare Needs | More emphasis on moisturization and anti-inflammatory care. | A hydrated, calm scalp reduces irritation and supports graft survival. |
| Follow-Up Frequency | Usually closer and more frequent check-ins. | Early detection of inflammation or plaques helps protect the results. |
Strong recovery is essential for long-term success. To understand the factors that shape a great outcome, explore Hair Transplant Success: The Key Elements Behind a Great Result.
Can a Hair Transplant Trigger Psoriasis?
A common concern among psoriasis patients is whether the procedure itself can activate new lesions. In some cases, a hair transplant can trigger a temporary flare, and this usually happens due to a well-known phenomenon in psoriasis called the Koebner response.
The Koebner phenomenon occurs when new psoriatic plaques appear in areas where the skin has experienced trauma. Because a hair transplant involves thousands of small incisions, patients with psoriasis have a slightly higher chance of developing a local flare if the condition is not well controlled.
Key points to understand:
- Risk is significantly lower when psoriasis is in remission. Stable skin responds far better to the micro-incisions used during FUE, Sapphire FUE, or DHI.
- Gentle surgical technique helps reduce trauma. Precise handling and minimal pressure make the scalp less reactive.
- Postoperative care influences flare risk. Proper moisturization, anti-inflammatory products, and avoiding scratching support a calm healing environment.
- Most flares, if they occur, are temporary. They usually resolve once inflammation settles and do not affect long-term graft survival.
Hair Transplant in Turkey for Psoriasis Patients With MCAN Health
Living with scalp psoriasis can make hair loss feel even more challenging, especially when flare-ups affect comfort, confidence, or styling. A hair transplant can still be a safe and effective option, but only when the condition is properly assessed and managed. At MCAN Health, we recognize that psoriasis requires a more personalized approach, beginning with a clear understanding of your scalp health, flare patterns, and long-term stability.
When you choose MCAN Health for your hair transplant in Turkey, you benefit from:
- Careful evaluation of psoriasis severity: Our specialists examine the scalp for signs of inflammation, plaque activity, and remission stability to determine whether surgery is appropriate.
- Tailored surgical techniques: We select between FUE, Sapphire FUE, and DHI based on the sensitivity of your scalp and the areas that require the most precision, reducing trauma and flare risk.
- Gentle, patient-focused implantation: Every step of the procedure is designed to minimize irritation and protect the skin, which is essential for patients with autoimmune conditions.
- Transparent, long-term guidance: We advise on timing, medical preparation, and aftercare strategies to help prevent flare-ups and support comfortable healing.
- Comprehensive care packages: From airport transfers and accommodation to follow-up support, your treatment journey is managed with clarity, comfort, and respect for your unique needs.
At MCAN Health, we combine modern hair restoration technology with an understanding of how conditions like psoriasis affect the scalp. Whether you are in remission and ready for treatment or still exploring your options, our team is committed to providing safe planning, natural results, and long-term support throughout your hair restoration journey.
 Unnatural Hair Direction After Hair Transplant: Causes, Fixes, and Re-Angling Options
Unnatural Hair Direction After Hair Transplant: Causes, Fixes, and Re-Angling Options  Widow’s Peak Hair: What Causes It and Can You Fix It with a Hair Transplant?
Widow’s Peak Hair: What Causes It and Can You Fix It with a Hair Transplant?  Hair Transplant Donor Area: Why It’s Critical for Natural and Lasting Results
Hair Transplant Donor Area: Why It’s Critical for Natural and Lasting Results